Third Party
Administrators (TPA’s)
TPA’s Provide Administrative Services for
Self-Funded Health Plans. We Do More
We Elevate the Member Experience

The “Four C’s” of TPA
Tribal Nations Health’s Care Advocates engage early and often with each and every plan member, to ensure a seamless member experience

Customization

Convenience

Compliance

Cost
Improve coding, reimbursement assurance, auditing, claim accuracy and compliance monitoring, all while saving time and costs
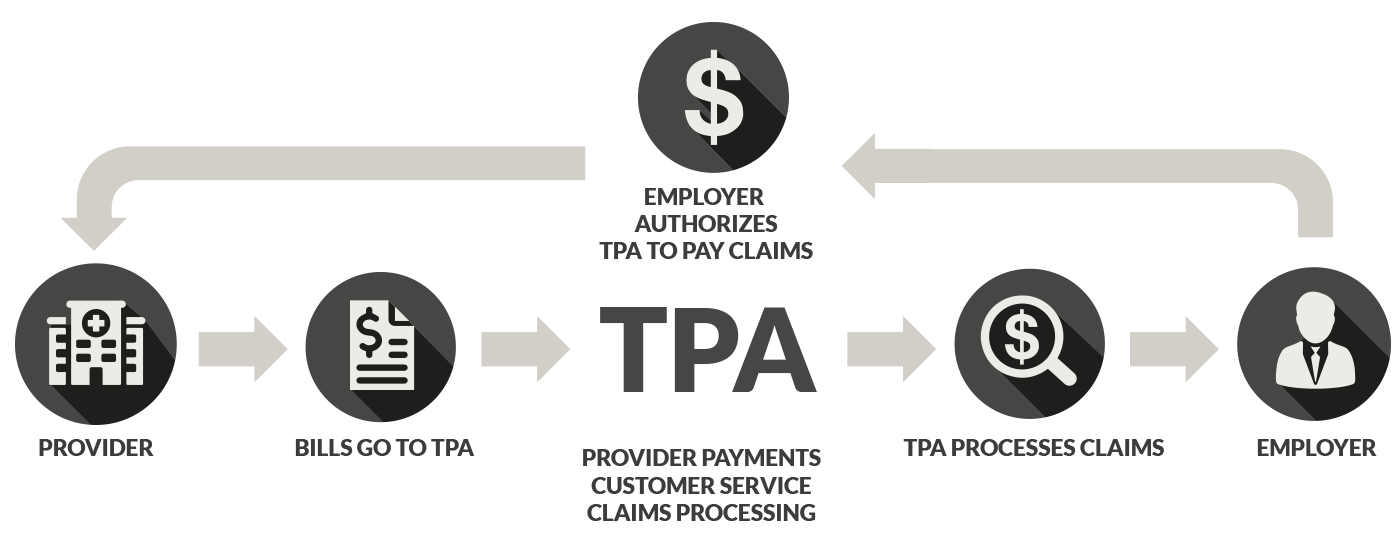
How TPAs Work
Tribal Nations Health’s TPA’s services drive your self-funded health plan toward consierge-level member care and profitability
Our services inform your members about the best provider fit, while negotiating with those same providers before your health care services are performed

Fully-Integrated Administrative Solutions
We’ve engineered quality service and consumer transparency in each of our plans, to deliver substantial cost savings and enhanced benefits for any size self-funded employer group
Full-Service Administration
Pharmacy Benefits
Tribal Nations Health delivers national accessibility with convenient, cost-effective options to prescription drugs. Our specialty drug programs help clients manage the prices of costly drug therapies.
Electronic Banking Solutions
Safe and secure banking and fiduciary solutions add value to any benefits package through consolidation, accuracy, and financial protection with a centralized electronic benefits payment service.
Ancillary Products
Ancillary products allow employers to offer their employees a complete benefits package based on the unique needs of their workforce, which include dental, vision, telemedicine, and other health care solutions.
Compliance Management
Tribal Nations Health always ensures that all benefits are in compliance with any applicable rules and regulations. You can rest easy that your plan is maintained within all state and federal regulations.
Provider Network Solutions
We provide a variety of provider network solutions that make it easy for employers to gain deeper insight into their plans. Our provider network plans can be customized using our preferred vendors or those of our clients.
Reporting and Analytics
Tribal Nations Health delivers advanced reporting and analytics tool for self-funded employers and producers. Our team helps provide insights into each plan and suggestions to support your plan goals.
Stop Loss Insurance
Stop loss insurance solutions provides cataclysmic protection for our self-funded medical and specialty prescription drug plans. Flexible options are available based on group size and budget.
COBRA Administration
COBRA administration can be complex and time-consuming. Tribal Nations Health has solutions to administer COBRA program benefits, including compliance, financials, and reporting on behalf of our clients.
Our TPA services differentiates themselves though built-in flexibility, member-centric care, and a custom-designed summary plan description, SPD (The Plan) tailored in excruciating detail to meet the needs of the plan sponsor
A Managed Care Solution that Works

Increased
Financial Control
Lower
Operation Cost

Benefit
Flexibility

Access to
Valuable Data
Close monitoring of each facet of your plan’s operational flow, allows us to optimize its potential. After all, it willl be designed specifically for you
Tribal Nations Health Helps Members Choose Quality Providers And Save On Their Out-Of-Pocket Costs, While Also Eliminating Balance Billing
Tribal Nations Health’s Member Advocacy program, ArrowCare, educates and guides members throughout the entire Value Based Pricing, “VBP” process. Our team of advocates determine which providers will accept VBP first. From there, they coordinate your care and act as your single point of contact for all payment and billing questions. ArrowCare educates and negotiates with health care providers before your health care services are performed. Our proactive process is paramount for eliminating the potential for financial liability—balance billing.
However, if a provider does send you a bill, ArrowCare will work on your behalf to get it resolved and keep your costs as low as possible.

Member and Patient Support
ArrowCare provides both pre-service and post-service patient support for members needing care under their value-based pricing program.
Schedule of Services
Once a case reimbursement agreement is established, our team of advocates are always standing at the ready to assist patients in scheduling.
Manage Certifications & Referrals
The ArrowCare team manages all certifications and pre-authorization referrals for the patient receiving care.
Pre-Service Negotiations
Patient advocates work directly with providers prior to perform any services and negotiate and agree to reimbursements defined by the plan benefits.
Re-Direct Provider Options
In rare instances when a provider does not accept the defined benefit reimbursement, ArrowCare will provide alternative options for care that will accept the defined.
Assistance with Balance Billing
In rare cases where patients receive a balance bill, ArrowCare’s experienced team will work directly with the provider to resolve the bill and relieve patients of any additional financial liability.
A Better Employer
Experience
Tribal Nations Health saves self-insured health plans money through creative benefit designs and provider reimbursement strategies. Our mission is to ensure both the financial health of the plan and the physical well being of its members. Healthy people are productive people.
A Better Employee Experience
TPA Checklist
Important services to look for when choosing a TPA. Here are the basics
- Access to real-time eligibility and claims history reports
- Accounting Support and Reconciliation
- Billing Services
- Eligibility Management & Communication
- Claim Adjudication and Auditing
- Case Management and Utilization Reviews
- Customer Service/Call Center
- Plan Setup and Summary Plan Descriptions
- Enrollment Materials and Member Education & Communication
- Identification Card Production
- Report Customization
- Coordination of Documentation for Stop-Loss claims
- Health Planning & Industry Expertise
